Early winter saw a subtle change that was not immediately apparent but was subtly altering patterns that families had relied on for years in North London’s school hallways. The sudden occurrence of absences, which spread slowly throughout classrooms, raised concerns that felt eerily similar to past public health crises that many had assumed were behind them.
Initially, parents reported common symptoms like fevers, coughing, and exhaustion, believing that rest would cure them in a few days. In the second week, however, physicians started verifying measles cases and spotting trends that pointed to a more serious issue that needed prompt, well-coordinated care.
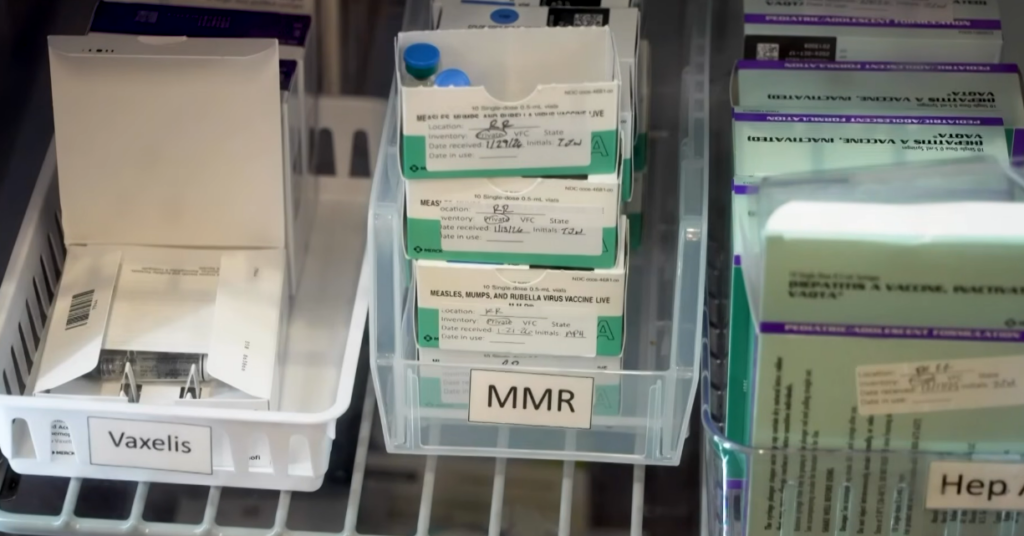
When at least seven schools and a nursery in Enfield reported confirmed cases, public health officials acted quickly, reaching out to families and creating very clear guidelines that were especially helpful in clearing up confusion. Their messaging focused on prevention, highlighting vaccination as a very effective defense that has been honed over decades of scientific advancement.
| Key Detail | Information |
|---|---|
| Location | Enfield and neighbouring boroughs, North London |
| Confirmed Cases | More than 60 children infected |
| Primary Setting | At least seven schools and one nursery |
| Most Affected Group | Children under 10 years old |
| Main Cause Identified | Low uptake of MMR vaccination |
| Hospital Impact | Some children required hospital care |
| Public Health Response | Emergency vaccination clinics and parental outreach |
The measles itself spreads with unnerving rapidity through shared surfaces, contact, and breath, appearing undetectable until symptoms manifest. Risk increases dramatically for children who are not fully immunized, allowing illness chains to spread gradually before intervention may stop them.
Working collaboratively with NHS teams, local authorities set up temporary vaccination clinics in schools, establishing access points that were unexpectedly inexpensive, completely free, and quite effective at getting in front of families. By functioning in well-known public areas, these clinics enabled parents to take prompt action and safeguard children without having to navigate convoluted healthcare systems.
As I stood outside one elementary school, I observed how parents spoke with remarkable patience and paid close attention to advice that might have sounded unneeded just a few weeks prior.
The outbreak shows where protection has deteriorated and how coordinated action may restore confidence, which is both concerning and an opportunity for health experts. Medical teams are utilizing well-established immunization programs in a methodical manner, increasing community resistance and expediting care delivery.
Fever, runny nose, and red eyes are common early symptoms that give way to the characteristic rash that is the clearest indicator of measles. The experience of turning daily activities into close observation and medical appointments can be quite upsetting for families who are not familiar with the condition.
Vaccination coverage has a particularly long-lasting significance in public health planning, offering protection that reaches entire communities as well as individuals. Maintaining high vaccination rates helps prevent outbreaks and protects vulnerable groups that are unable to get vaccines on their own.
However, vaccine uptake has significantly decreased in some London boroughs over the last ten years due to a combination of misinformation, scheduling conflicts, and changing public attitudes. Even though it started off quietly, this slow transformation put systems meant to stop infections from reoccurring in a test environment.
By acting swiftly and forcefully, public health officials have shown a particularly creative strategy, taking immunization campaigns inside schools and interacting with parents in a compassionate rather than critical manner. Their communication-and accessibility-based approach has been incredibly successful in persuading families to change their minds and adopt preventative measures.
In addition to being individual cases, children recovering at home now serve as a reminder of the community’s resilience and vulnerability. Teachers and students alike are reminded by their absence from class that maintaining one’s health is an ongoing duty rather than a given.
While preserving stability for children, the outbreak has changed the daily routines of teachers by incorporating health monitoring in addition to academic instruction. Their efforts demonstrate a dedication that is both incredibly pragmatic and subtly comforting, as they swiftly adjust to changing conditions.
As well, parents have adapted, scheduling checkups, reviewing immunization records, and having more serious conversations about illness choices. By performing these actions, kids actively support containment efforts and improve safety for their classmates, neighbors, and own children.
Since local immunization clinics started, attendance has significantly increased, indicating a greater knowledge and readiness to take positive action. Every consultation is a tiny but significant step in strengthening protection that is both socially necessary and scientifically validated.
Although they are cautiously optimistic, public health experts point out that when communities work together, measles outbreaks may be efficiently suppressed. Their assurance is backed by decades of data demonstrating vaccination’s exceptional efficacy in averting widespread disease.
Both a challenge and a turning moment, the epidemic in North London has brought formerly regular public health procedures back into the spotlight. Communities can guarantee that future classrooms are places of learning rather than worry by boosting vaccination rates.